2.6 - Documentation

Which documentation system do you use?
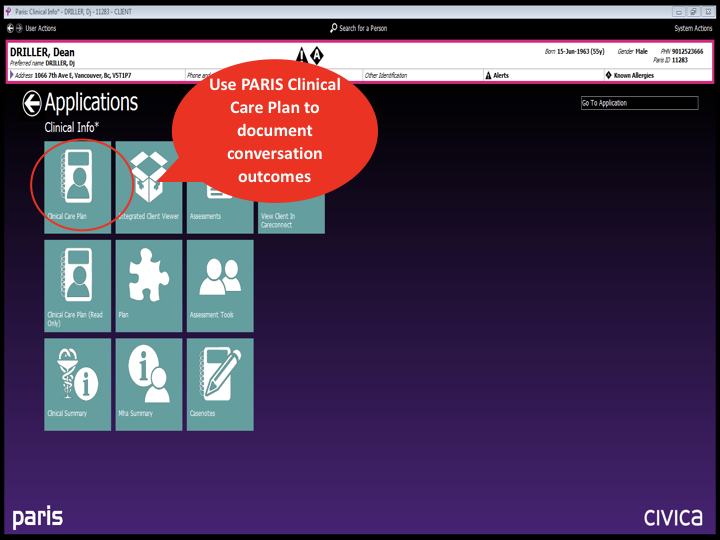
PARIS

If you need a refresher on how to enter clinical care plans, please access the online education Paris 6 VCH Clinical Care Plan (ALL) on the LearningHub.
Download the PARIS Documentation Template from the IPACE Website under Resources for Download, or from your shared drive at your respective teams. All IPACE documentation follows PARIS Guidelines. Please refer to the PARIS User Help or your local Resource Nurses if you have any PARIS related questions.
Step 1.
Step 2.
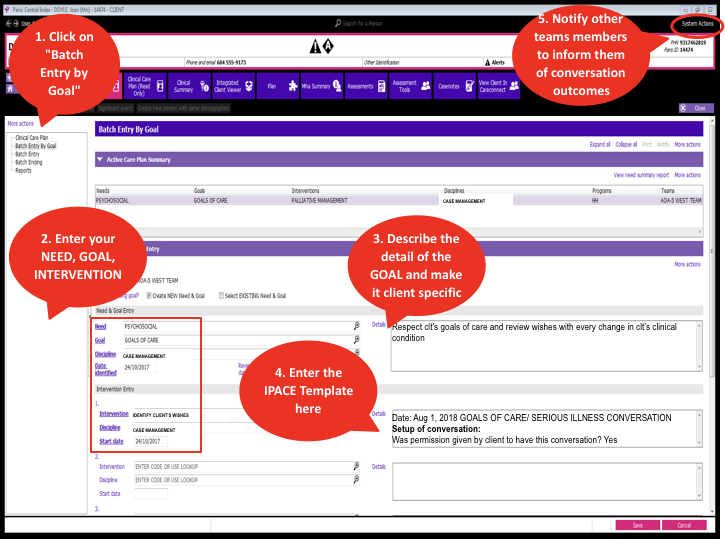
Summary
Profile EMR

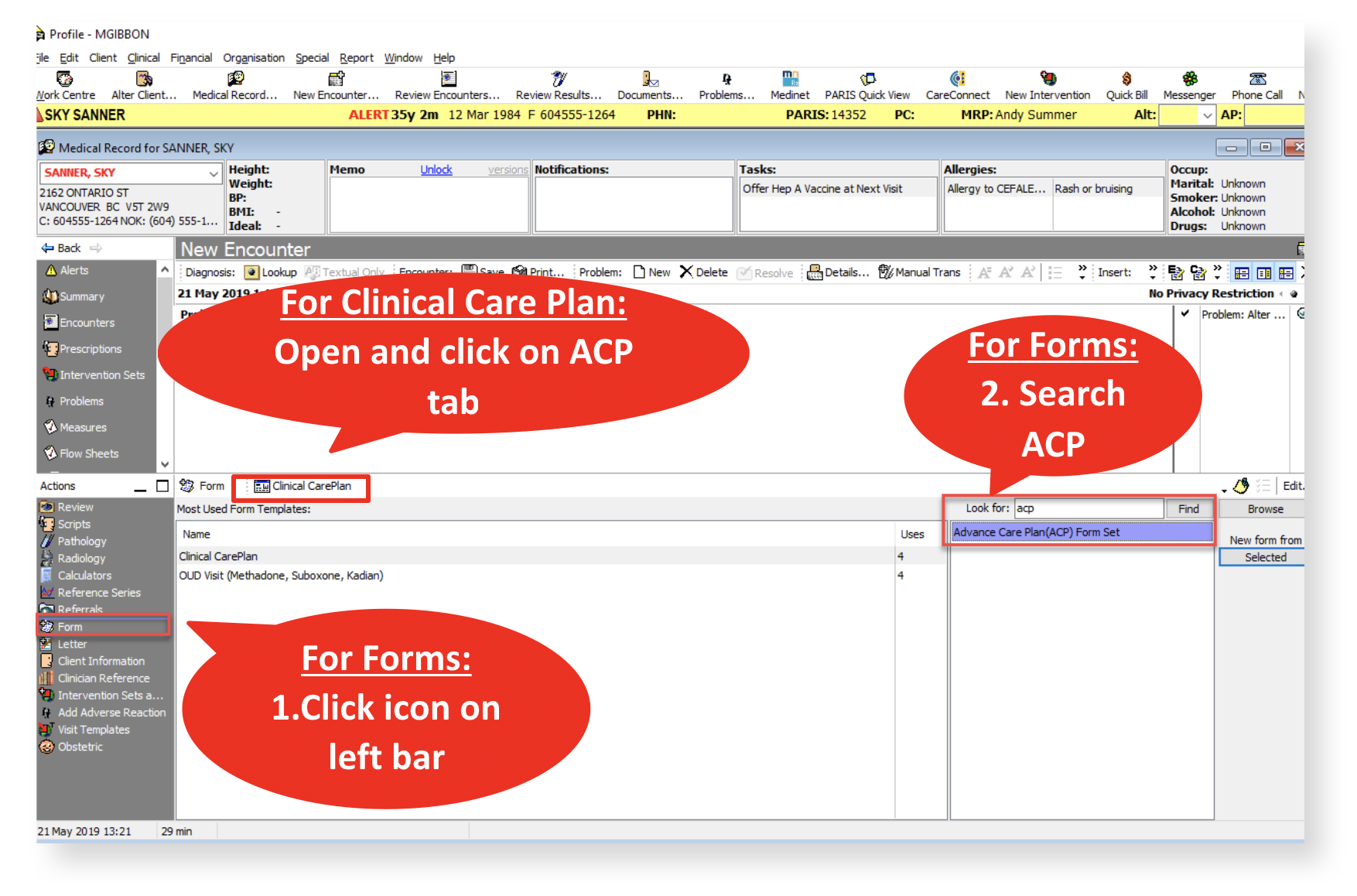
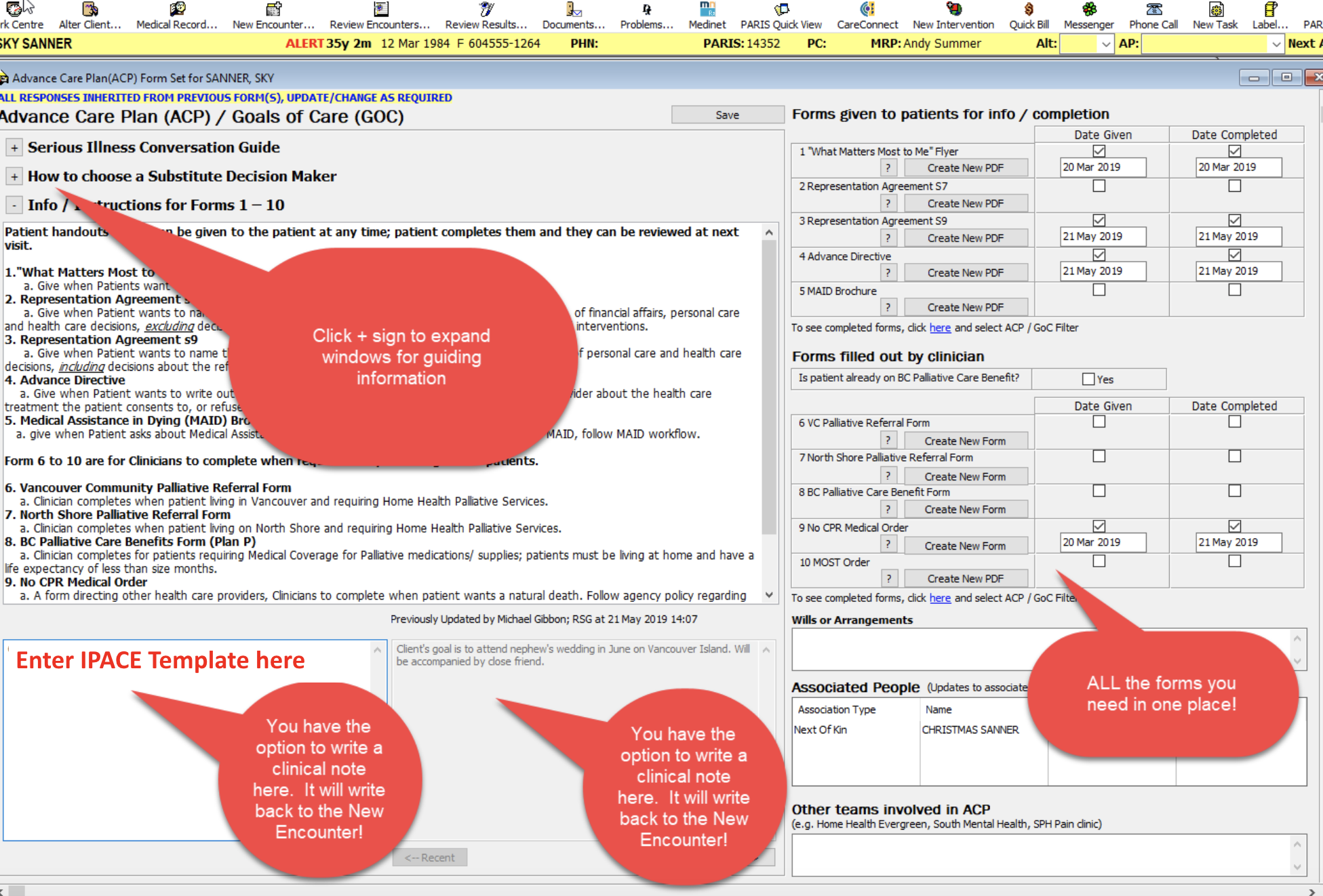
Download the Profile EMR Documentation Template from the IPACE Website under Resources for Download, or from your shared drive at your respective teams. Please refer or your local Resource Nurses/ Educators if you have any Profile EMR related questions.
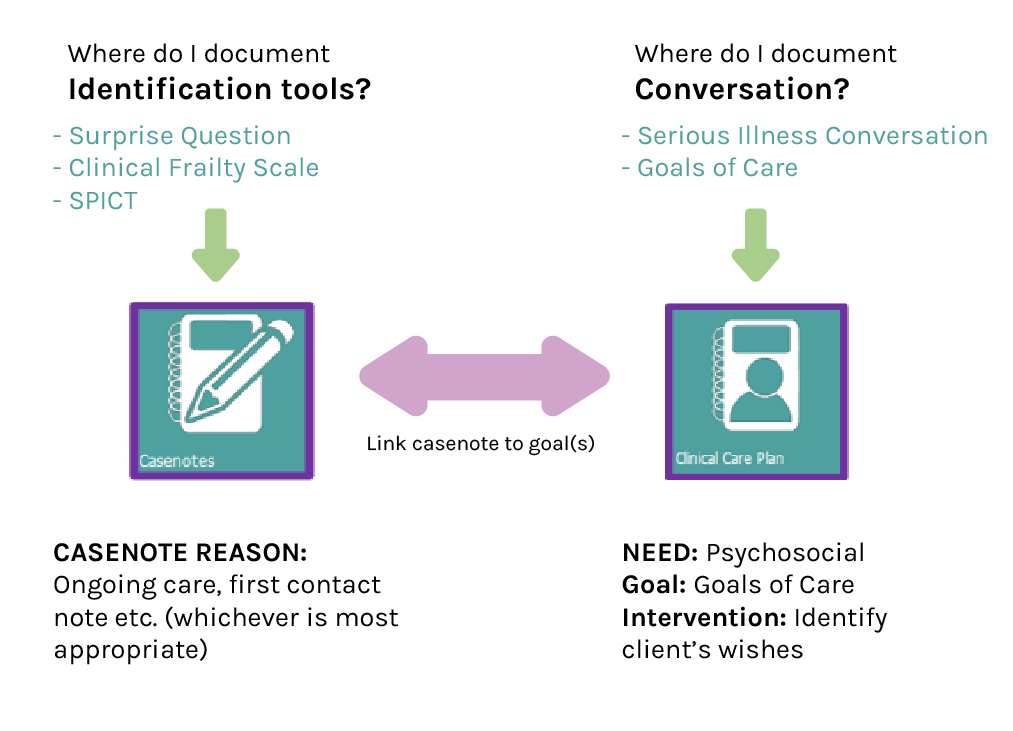
There are 2 places to document in Profile EMR for IPACE
- Problem List: This information is shared into Care Connect
- Advance Care Plan: This can be accessed through Clinical Care Plan or Forms
1. Add to problem list

2. Advance Care Plan (ACP)
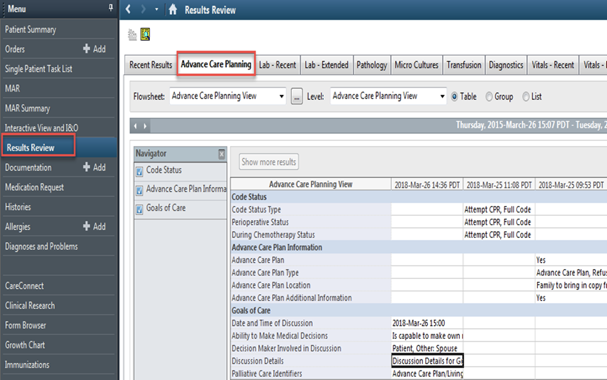
Cerner/CST

You can document GOC conversations in Cerner through several pathways, depending on your user profile:
Results Review — Advance Care Planning
Patient Summary — Handoff Tool
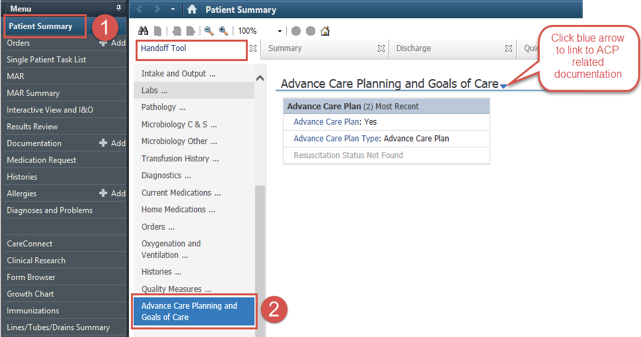
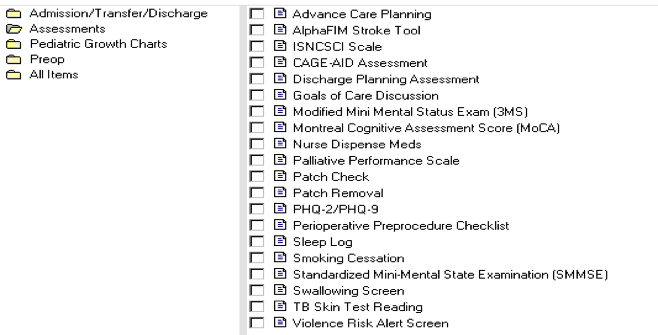
Ad Hoc Forms (Assessment -> Goals of Care Discussion)
Paper Charting

All discussions that disclose patient wishes, values, and fears or anything related to advance care planning should be documented in the Advance Care Planning/Goals of Care (ACP/GOC) discussion record (VCH.0109). This is the same interdisciplinary document where the team would document the identification of a patient who would benefit from a Serious Illness or Goals of Care Conversation, including any tools used to identify the patient (please see module section 1.7 for details on Identification). Conversations must be documented here rather than in discipline-specific progress notes so that they can be easily viewed by all members of the interdisciplinary team. As a reminder, this form can be found either:
- A) Inside the green sleeve behind the MOST. Staff may wish to place a note in front of the MOST to alert others that the ACP/GOC discussion record has documentation on it, and is behind the MOST, or
- OR B) Directly behind the green sleeve.
Use narrative or point-form to record any conversations around goals, wishes, expectations, fears, worries, or Advance Care Planning, including discharge planning and follow-up.
- Capture both formal and informal discussions, including hallway or bedside conversations, family meetings, or phone calls with loved ones or staff from other institutions (e.g. case managers from community, long-term care providers).
- If only one question/concern is discussed, document just the answer to that question.
- Include any major updates around new diagnoses, information that was shared with the patient/family, and treatment options that are being considered.
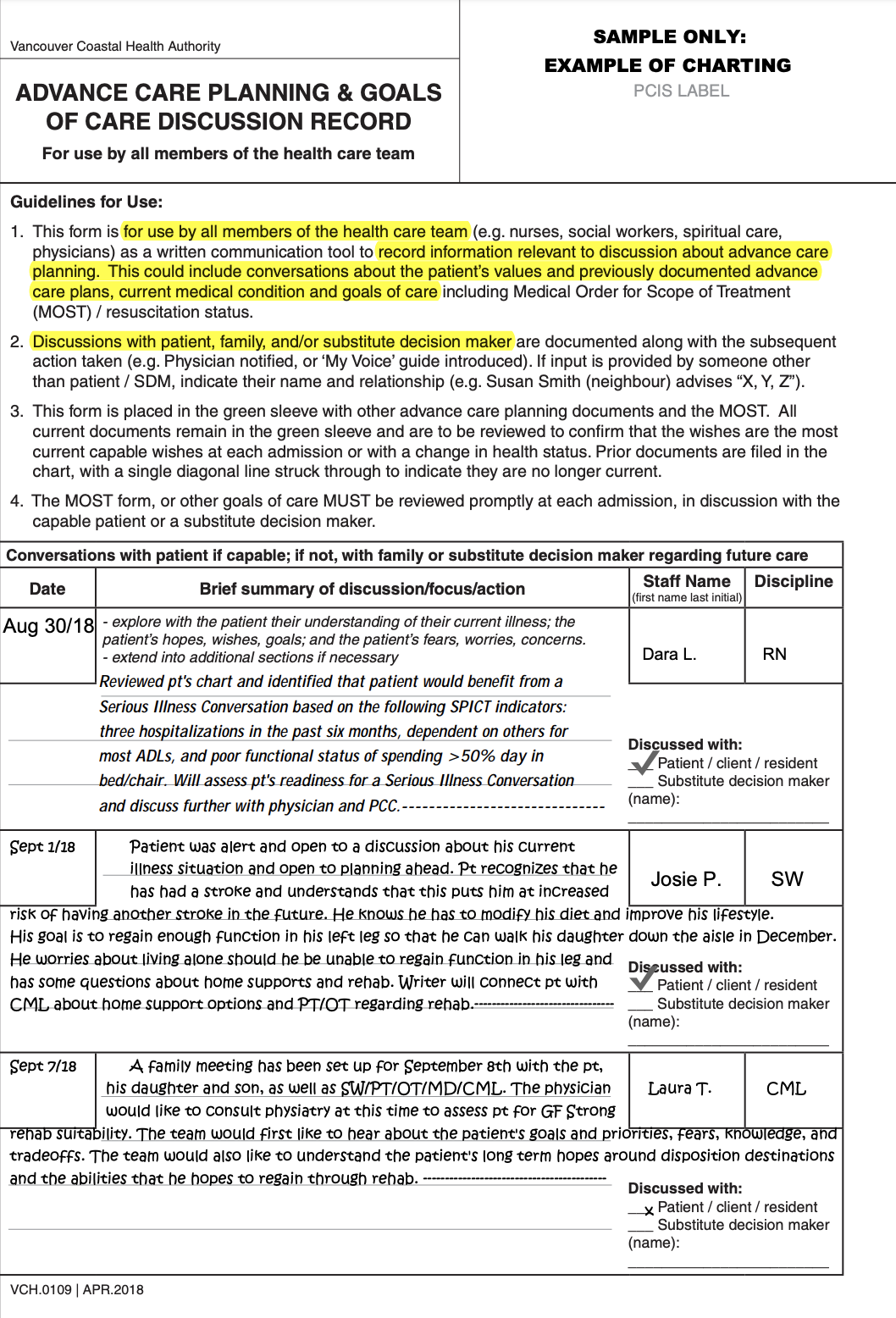
In order to avoid double-charting:
- In discipline specific notes, write "Please see the ACP/GOC discussion record for documentation of ____ (SIC, GOC, discharge concerns, etc...)" No further documentation is required here.
Other Documentation Systems (Long Term Care and Assisted Living)

All clinicians within a given team document goals of care in a central location so that any team member can easily find the documented goals of care.
Clinicians should use their clinical judgement about whether the documented information should be urgently shared with other team members.
Examples:
- Patient is reconsidering surgery → inform physician
- Patient has discharge concerns or altered plans → inform discharge planning teams
- Patient has had a complex symptom exacerbation and has made an informed decision to stay at home and focus on a quality of life → inform team and physician
The process for sharing information urgently will be up to the program/unit's own workflow.
Please refer to your clinical lead/educator or contact the Regional Palliative Approach to Care Education Team listed under Resources.
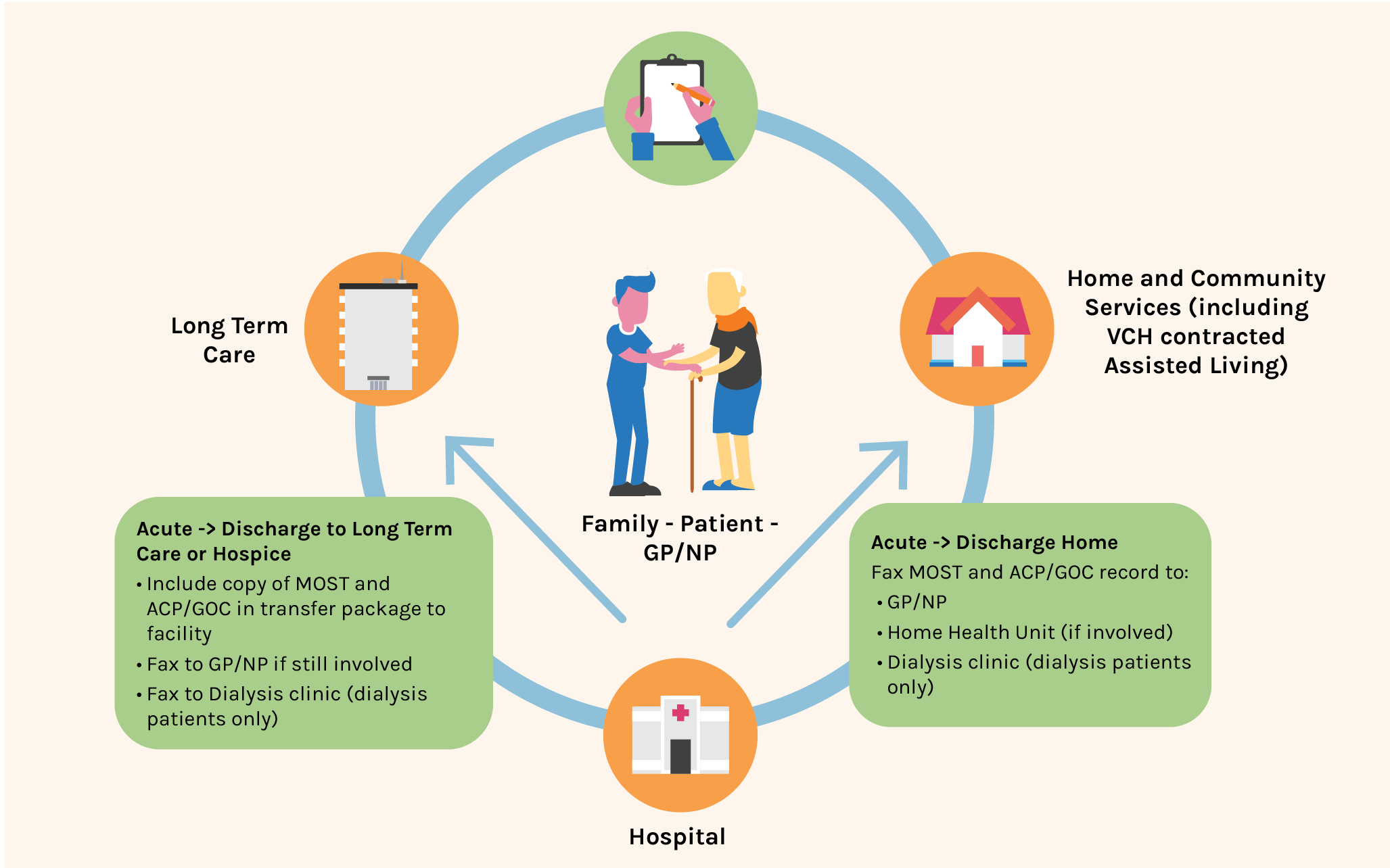
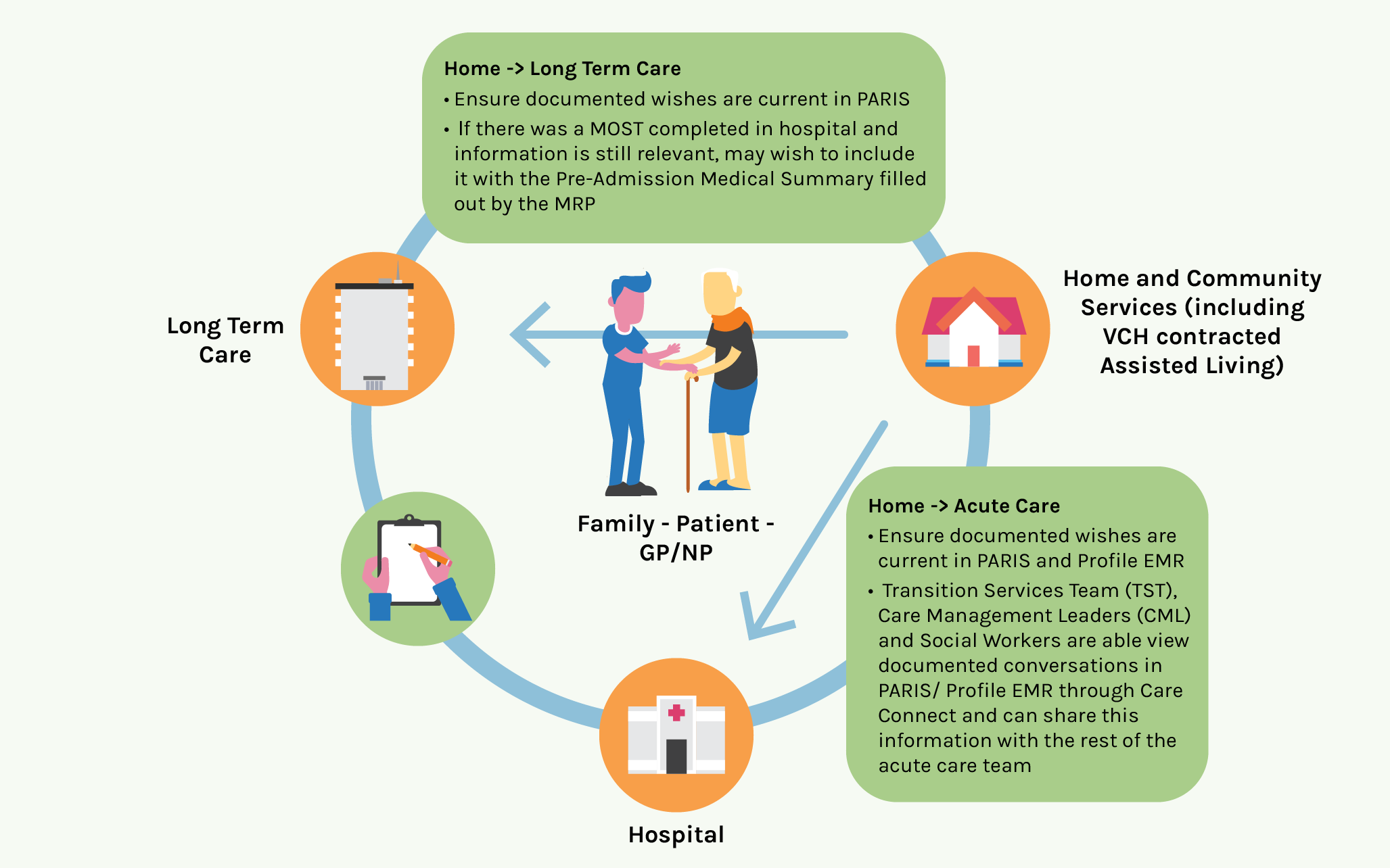
Communication
Patients will require a variety of services during the course of their illness. Ensuring a patient's wishes are communicated across the continuum of care allows teams to prioritize care according to people's wishes.
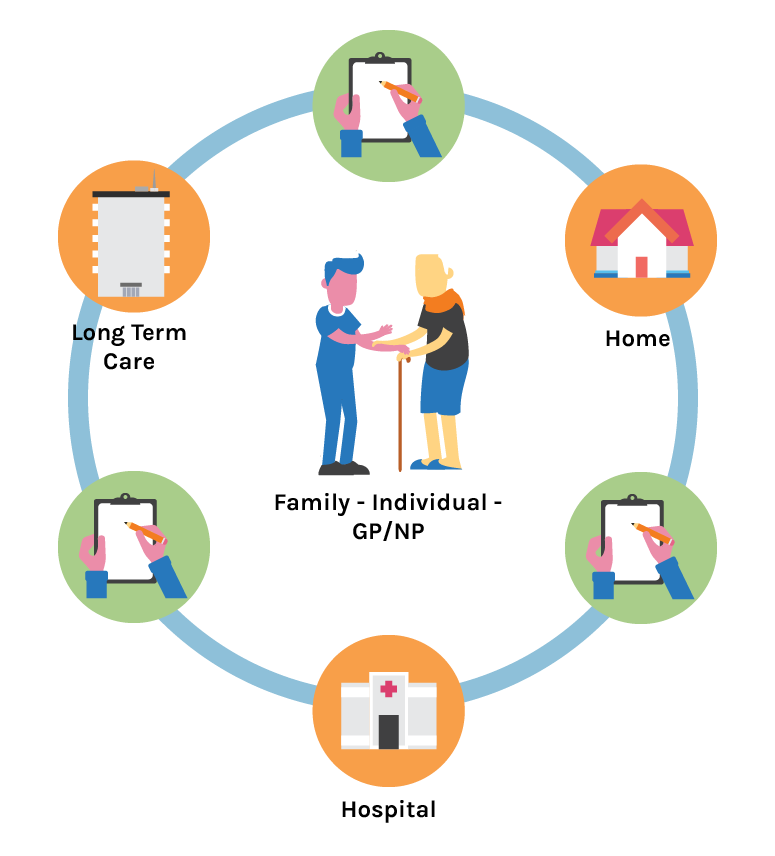

How does information get shared at care transitions?
CareConnect supports continuity of care as patients move across programs and services. This view-only system allows electronic health record users to view a limited amount of patient information documented in another electronic documentation system. This includes documented conversations for certain programs and teams.